Image BruceBlaus
Hysterectomy
What is a hysterectomy?
Hysterectomy is the surgical removal of the uterus. There are several reasons why this may be required. These include benign conditions such as fibroids, endometriosis, excessive menstrual bleeding, prolapse and malignant ones such as cancer of the ovaries, uterus or cervix.
To remove the uterus the surgeon needs to tie or ligate all the vessels and ligaments that provide blood supply and support to the organ. This is done following precise surgical technique.
Once all the vessels and ligaments have been ligated, the uterus is removed. In most cases, the cervix is also removed (“total hysterectomy”).
Hysterectomy procedures
There are four main ways to perform a hysterectomy depending on the way the surgeon gains access to the inside of the abdomen: vaginal, abdominal, laparoscopic or robotic. Sometimes a combination of routes can be used.
Abdominal Hysterectomy
The abdominal hysterectomy requires a 10 to 15 cm surgical incision, similar to the one used for a caesarean section. The surgical incison goes through all the layers of the abdominal wall. Once the abdominal cavity is reached, the surgeon goes through a number of distinct surgical steps to ligate the blood vessels and ligaments that are attached to uterus. The uterus is then freed and removed. The hysterectomy can be subtotal, when the body of the uterus is removed and the cervix remains or total, when the cervix is also removed.
This is the less preferred option nowadays and is only used when a vaginal or laparoscopic hysterectomy is not possible, usually in the case of very large uteruses as can happen with uterine fibroids.
Vaginal Hysterectomy
A vaginal hysterectomy, when possible, is a good option. As the name says, the procedure is done through the vagina and does not require any abdominal incisions. The same blood vessels and ligaments are secured and the uterus is removed through the vagina. A vaginal hysterectomy is always total and includes removal of the cervix. Post-operative pain is less and recovery is faster than an open abdominal hysterectomy.
Laparoscopic and Robotic assisted hysterectomy
Laparoscopic and robotic assisted hysterectomies are minimally invasive options that follow the same principles and similar surgical steps as the open abdominal procedure. However, the instruments used and the way the vessels and pedicles are secured are somewhat different.
With the laparoscopic and robotic procedures, the operation is performed through 4 small incisions of around 0.5 cm each. A camera is inserted in the abdomen through one of the incisions and the surgeon sees the internal organs on a screen while operating with long thin instruments.
In the traditional laparoscopy the surgeon holds the instruments. With the robot, the instruments are attached to robotic arms which are then controlled by the surgeon seating at the nearby console.
After a laparoscopic or robotic assisted hysterectomy, most women go home after 1 or 2 days and return to work within 3 weeks.
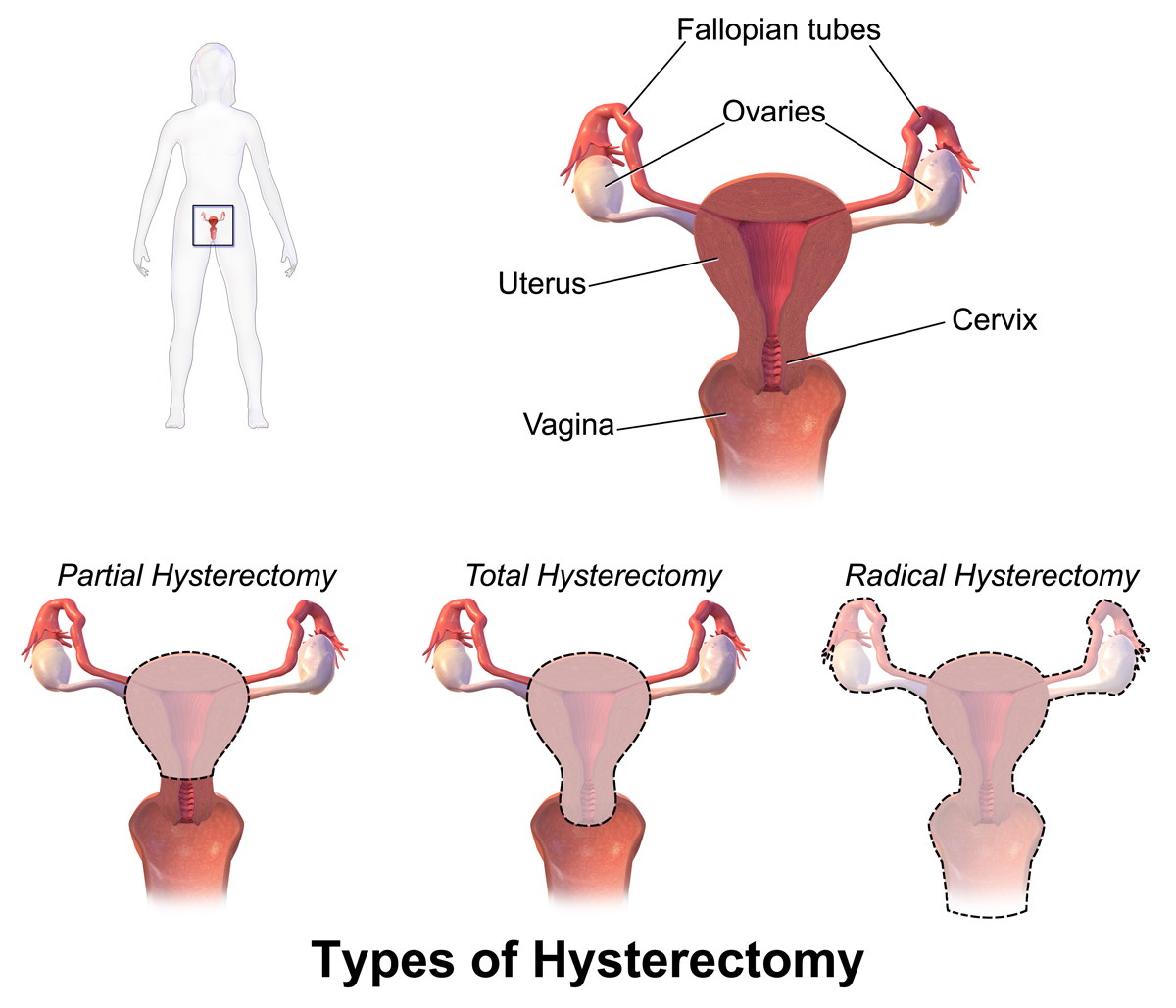
Different types of hysterectomy
Total hysterectomy
Involves the removal of the body of the uterus and the cervix.
Subtotal hysterectomy
Involves the removal of the body of the uterus while preserving the cervix.
Hysterectomy and Salpingo-oophorectomy
Involves the removal of the uterus as well as the ovaries (Oophora) and Fallopian tubes (salpinges)
Radical hysterectomy
Done in cases of cancer, a radical hysterectomy includes the removal of the uterus (cervix and body), fallopian tubes and ovaries as well as uterine ligaments (round, broad, cardinal and uterosacral ligaments) and the top third of the vagina. Removal of the pelvic lymph nodes is also commonly done. The aim is to remove all areas that can contain cancerous cells with a margin of safety.
Frequently Asked Questions
What are the reasons that may require a hysterectomy?
Some diseases of the uterus can cause severe symptoms. Many of those can be treated with medication and other conservative measures. When these measures fail, consideration can be given to removing the uterus. Some conditions are benign, that is not cancerous. They include: uterine fibroids, endometriosis, excessive menstrual bleeding (menorrhagia) and pelvic organ prolapse.
Malignant condition mean cancer of the uterus, cervix and ovaries.
How do I know if I need a hysterectomy?
If you have been diagnosed with ovarian or uterine cancer, your treatment will most certainly include a hysterectomy and possibly removal of both ovaries. These situations tend to be quite determined and there isn’t really much of an option as most cases require removal of the tumour and the organ affected.
If the case of the benign conditions mentioned above, the process is different. It involves consideration of conservative measures that could control symptoms without requiring surgery. These could be in the form of hormones and other medications, hormone containing IUDs (Mirena, Kyleena), endometrial ablation, etc.
Also, the benefits of the surgery have to be weighed against potential risks and complications of the operation.
How urgently do I need the hysterectomy surgery done?
If a hysterectomy is necessary because of cancer, usually the sooner the better.
All other conditions are not that urgent and most times a hysterectomy can be delayed if necessary in order to consider other options and/or choose the best time for surgery. One exception, are cases of very severe bleeding (such as with fibroids) where the woman’s health can be at risk.
Are the ovaries removed during a hysterectomy?
No. A hysterectomy involves only the removal of the uterus and not the ovaries. In some cases, the ovaries and fallopian tubes also need to be removed and this is usually either because of cancer or, less commonly, very severe endometriosis. If that is the case, the operation will be called hysterectomy + salpingo-oophorectomy.
What is the difference between a vaginal, abdominal, laparoscopic and robotic hysterectomy?
The main steps of all four procedures are similar and involve ligation of the arteries that bring blood to the uterus and ligaments that hold it in place. The terminology relates to the route of access for the operation. As the names suggest, a vaginal hysterectomy is done through the vagina with no abdominal incisions, an abdominal hysterectomy is done through a 10 – 15 cm cut on the abdomen similar to a caesarean section and a laparoscopic and robotic hysterectomies, also called keyhole surgeries, are done through four 0.5 cm incisions on the abdomen. The instruments used in each type of operation are different to suit each mode of access.
The large incision on the abdomen for an abdominal hysterectomy usually means more post-operative pain and a longer recovery period when compared to a laparoscopic, robotic or vaginal hysterectomy.
What are the benefits of having a hysterectomy?
The benefits of a hysterectomy are directly related to the resolution of the symptoms caused by the condition requiring the removal of the uterus.
Some examples are pain and bleeding caused by endometriosis and adenomyosis as well as bleeding and pressure symptoms caused by fibroids. In the case of cancer, a hysterectomy may be necessary as part of the treatment to remove the tumour.
The decision to have surgery is taken by comparing the potential benefits to the risks of having the operation as well as the benefits of other treatments that do not involve an operation.
Operations performed with a good indication on well prepared and informed women show high post-operative satisfaction rates.
What are the risks involved with a hysterectomy?
Every surgical procedure and medical intervention carries risks. Some of these risks are inherent to all admissions to hospital and surgical operations while some are particular to the specific procedure being undertaken.
New processes and safety measures are always being adopted to minimise risk. Fortunately, nowadays surgery is mostly safe and complications are low.
The main risks associated with hysterectomies are:
Excessive bleeding: the risk of losing too much blood during the operation to the point of requiring a blood transfusion is around 1 in 500 cases.
Infection: An infection can happen on the surgical site in the pelvis where the uterus is or on the surgical wounds in the skin. A single dose of antibiotics is given during the operation and this, in addition to sterilisation of instruments and aseptic surgical technique, is usually enough to prevent surgical infections. When it happens, additional antibiotic treatment and, in some cases, further admission to hospital may be required.
Damage to surrounding organs: during a hysterectomy there is potential risk of damage or injury to one of the nearby organs namely the bladder, bowel, ureters (the tubes that bring urine from the kidneys to the bladder) or one of the large blood vessels (arteries or veins). Although rare, these can cause serious problems if unnoticed at the time of the operation as faeces and urine can leak into the abdomen on the days following the surgery. If diagnosed during the operation, small injuries can be fixed and do not tend to cause long term issues.
Discussion of surgical risks and complications are part of the informed consent you will sign before your hysterectomy and you should take the opportunity to discuss them with your doctor.
The discussion should involve the possibility of using alternative treatments other than surgery as well as weighing the benefits from having the surgery when compared to the risks of the procedure.
Is a laparoscopic hysterectomy riskier than an open abdominal hysterectomy?
No. When the operation was first performed in the 1990s a higher incidence of organ damage and bleeding was reported. This is now believed to have occurred mainly because of surgeon's inexperience and introduction of the new method.
Nowadays, in experienced hands, when compared to an open procedure, a laparoscopic hysterectomy generally means less bleeding, less pain, faster recovery, faster return to physical activities and to work and better cosmetic results. Several studies comparing laparoscopic, vaginal and abdominal hysterectomy show the laparoscopic and vaginal procedures as the better options.
Will I put on weight after a hysterectomy?
No. There is no relationship between a hysterectomy and weight gain.
If I have a hysterectomy will I enter menopause?
After a hysterectomy you will no longer have periods. Nevertheless, if your ovaries have not been removed you will not be in menopause and will continue to ovulate, produce hormones and experience hormonal cycles.
Some studies showed that women who have a hysterectomy can experience hormonal menopause six to twelve months earlier when compared to women who did not have the uterus removed. On average, one should expect to reach menopause, i.e., reduction in ovarian hormones and discontinuation of ovulation, around the same age they would if they did not have a hysterectomy.
Will the hysterectomy affect my sexual pleasure?
This in an uncertain area because of the different reasons for which hysterectomies are performed, different ways it is performed, the large role played by emotions and culture over sex and women's attitudes towards the uterus. Sexual pleasure and orgasm should remain by and large the same as before. Most sexual stimulation happens on the lower (most external) third of the vagina and the clitoris and these are not altered by a hysterectomy. There are cases of women who report changes in their sexual life after a hysterectomy. These can be for the worse or the better.
Improvements tend to happen when the hysterectomy was performed for reasons that were interfering with sex in the first place such as pain or bleeding. Some women also report becoming more confident knowing that they are no longer at risk of falling pregnant. Studies that looked into the effect of hysterectomies on sexual life found that the most satisfied women are the ones who had good reasons to have the hysterectomy and who had good pre-operative discussion, counselling and expectations.
A few physiological considerations include: Some women experience short repeated uterine contractions after orgasm and these tend to disappear after the hysterectomy. Some women experience short repeated vaginal contractions after orgasm and these tend to remain the same. Vaginal lubrication is mostly secretions from the vaginal wall during arousal and it also remains the same.
Will the hysterectomy change my desire for sex?
Your sexual desire (libido) should stay the same as before the hysterectomy. In some women, the removal of pain and heavy bleeding may increase sexual desire. The most common causes of reduction in libido are stress, fatigue, and fear of pain with intercourse. A hysterectomy may interfere with sexual desire to the extent that it interferes with those factors. In most cases there is no change.