Endometriosis
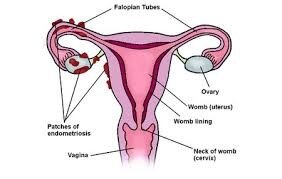
Endometriosis is the presence of endometrium (the tissue that lines the uterine cavity) outside the uterus.
The uterus has two main types of cells; muscular cells that make the uterine walls known as myometrium and glandular cells that make the lining of the uterine cavity known as endometrium.
Endometriosis is a condition where patches of endometrial cells grow in other organs in the body, most commonly in the pelvis near or over the back of the uterus, the ovaries, bladder and bowel.
Endometrial cells have a very specific function, which is to provide the grounds for a fertilised embryo to attach at the beginning of the pregnancy. The hormones produced by the ovaries during the menstrual cycle stimulate these cells and make them grow in size and number, as well as change their function over the cycle. When the woman doesn't fall pregnant, these cells die and shed causing the menstrual flow.
The areas of endometrial tissue outside the uterus (the endometriotic lesions) respond to the ovarian hormones of the menstrual cycle in the same way as the endometrium inside the uterus. Like the endometrium in the womb, the lesions thicken and swell with blood in order to prepare for a possible pregnancy. This swelling causes inflammation which in turn can be painful.
It is not fully understood why some women develop endometriosis and others don't. There are several theories that explain the disease. The most accepted one is retrograde menstruation: when a woman is having her period, small amounts of menstrual blood flow backward through the Fallopian tubes into the abdominal cavity. This blood contains endometrial cells that shed during menstruation. Some of those cells attach and implant onto the pelvic and abdominal cavities. They then start to grow and multiply developing into patches or nodules of endometriotic tissue.
Endometriosis is known to run in families. Although a gene that causes endometriosis has not been isolated, the sister or the daughter of a woman with endometriosis is seven times more likely to have the disease than someone who does not have a first degree relative with the disease.
Endometriosis Symptoms
Endometriosis symptoms may vary and the severity of symptoms doesn't always correspond to the amount of disease found.
Pain
Pain is the most common endometriosis symptom. Women who have endometriosis commonly experience pelvic, abdominal and lower back pain. The pain usually has a cyclical nature and is more severe on the days leading to and during a woman's period. Pain can also be present during or after sexual intercourse, and in cases where the disease implants on bowel or bladder, bowel movements or passing urine can be uncomfortable.
Irregular bleeding
Changes in the menstrual pattern can be the first sign of endometriosis. These are not always accompanied by pain. The most common presentation is bleeding outside the normal period days.
Infertility
Infertility is present in 30% of women who have endometriosis.
Women with cyclical pain and infertility should be investigated for endometriosis. In addition, even in the absence of pain, when no other cause of infertility is apparent, endometriosis should be considered.
Other symptoms
Other symptoms are less specific but sometimes can be the first signal that a woman has endometriosis. They include bloating, diarrhoea, constipation, increased urinary frequency, tiredness and/or fatigue.
All of these endometriosis symptoms can have other causes so it is important to investigate other possible medical conditions.
→ Learn more about Endometriosis Signs & Symptoms
Diagnosing Endometriosis
Laparoscopy
The best way to diagnose endometriosis is through a laparoscopy, also known as keyhole surgery, where a camera is inserted into the abdomen through a small incision near the umbilicus.
Endometriotic lesions can then be seen by the surgeon and samples can be taken and sent to pathology. Histopathologic (biopsy) evidence is the definitive confirmation of the disease.
Other tests can suggest the presence of the disease, but to date there are no non-invasive ways of making an unequivocal endometriosis diagnosis.
Ultrasound
Ultrasound is the principal mode of imaging used for the pelvis as it is very effective to assess the uterus and ovaries. However, most endometriotic lesions are not visible on ultrasound. The ultrasound can show endometriosis in cases where there is an endometriotic cyst on one or both ovaries (endometrioma) and/or when there are disease forming nodules in the pelvis.
When looking for endometriosis, it is very important to have the ultrasound done by a doctor trained in the diagnosis of the disease.
Magnetic Resonance Imaging
MRI is another useful resource to assess endometriosis. Similar to the ultrasound, it does not show superficial endometriotic lesions, but can be very useful to assess more severe forms of the disease when there are ovarian cysts or nodules affecting the vagina, the rectum or the bladder.
Blood tests
There has been a lot of research trying to find a blood test for endometriosis. To date, there is no reliable blood test to diagnose the disease.
CA 125 is a protein that is found in greater concentration in tumour cells than in other cells of the body. Women with ovarian cancer can have high levels of CA 125 in the blood.
Although some women with endometriosis also show high levels of CA 125 in the blood, the test is not reliable and is not routinely used to diagnose the disease.
Unfortunately, there still isn’t one single test that can reliably diagnose endometriosis and definitive diagnosis of the disease requires a laparoscopy.
The decision to do a laparoscopy is made after considering the symptoms, physical examination and ultrasound results.
→ Learn more about Diagnosis of Endometriosis
Treatment and Follow Up
Not every case of endometriosis requires treatment.
Endometriosis is a benign disease, that is, it is not cancer and, in many cases, does not cause major harm.
The two main reasons to try to make a definitive diagnosis of endometriosis and to treat it are pain and infertility.
The treatment can be surgical, by removal of endometriosis implants, nodules or cysts during the laparoscopy and/or with medication. There are several options for medical treatment. These include hormonal contraceptives and drugs that block ovarian function.
Other options include pain killers, natural therapies and physical exercise.
Endometriosis can be a chronic recurrent condition requiring more than one operation and many years of follow up. It often affects young women before they have had children and treatment aims at preserving fertility by preserving the reproductive organs, i.e., uterus, ovaries and fallopian tubes.
→ Learn more about Endometriosis Treatment & Surgery
Frequently Asked Questions
Is all endometriosis the same?
There two main types of endometriosis; superficial and deep infiltrating. Superficial endometriosis describes lesions over the peritoneum, a thin membrane that covers the pelvic and abdominal organs. Deep infiltrating endometriosis presents as nodules which infiltrate the pelvic organs, most commonly the uterine ligaments, vaginal septum, bladder and rectum.
Furthermore, there are different degrees or levels of disease depending on the amount of endometriosis seen, the number of organs involved and the degree of scarring and internal adhesions. Endometriosis may be simply classified as mild, moderate or severe, or in more detail as Stages 1 to 4.
Lastly, endometriosis can be asymptomatic. In the absence of symptoms, women won't know that they have the disease.
How do I know if I have endometriosis?
You can't know whether you have endometriosis until you have seen a specialist who makes the diagnosis. A definitive diagnosis usually requires a laparoscopy. You can suspect that you have endometriosis if you have any of the symptoms described above or if you had an ultrasound or MRI reporting the disease.
Do I need to see a doctor if a close relative was diagnosed with endometriosis?
Not necessarily. Having a family history of endometriosis increases your risk of having the disease, but doesn't mean that you will definitely have endometriosis. You should only see a doctor if you have symptoms.
I have been diagnosed with endometriosis. Will I ever be able to fall pregnant?
It's impossible to respond with certainty as every case is different and we don't know until you try to conceive. The answer is most likely yes, as two thirds of women who have endometriosis still fall pregnant naturally and the others usually respond well to fertility treatment.
I was treated for endometriosis in the past and now I seem to have the same symptoms again.
Endometriosis is a chronic disease and the conditions that made it occur the first time are usually still present. Recurrences are therefore common. On average, one in three patients who had a laparoscopy for endometriosis will require a repeat procedure within five years.
Is endometriosis contagious? Can I get it from someone else?
No. Endometriosis is not a transmissible disease. You don't get it through sex or contact with other people that have the disease.
Can I treat endometriosis with Natural Therapies and Complementary Medicine?
None of these modalities will cure endometriosis, but they all have been shown to help manage the symptoms.
Acupuncture, herbal therapy, massage techniques, exercise under the guidance of a trained professional, good nutrition, and adopting a generally healthy lifestyle, while not a cure for the disease, may significantly improve the symptoms.
Can children and post-menopausal women have endometriosis?
Usually not. Endometrial tissue grows under the influence of ovarian hormones. These are present after puberty and stop around menopause. Although not impossible, it is very unlikely that a girl who has not started her periods or a woman who has reached menopause will develop endometriosis.
Is there a cure for endometriosis?
There is no definitive cure for endometriosis, but there is treatment. Surgical treatment aims at removing the endometriotic lesions. Medical treatment aims at alleviating the symptoms. Different women may require different treatments or a combination of treatments.
Will I cure my endometriosis if I fall pregnant?
No. Most women will have a reduction of symptoms during pregnancy, but it may recur after childbirth and breastfeeding. Falling pregnant is a good thing as it removes one of the anxieties about the impact of endometriosis on fertility. Also, after completing the family, other more aggressive surgical options can be considered if required to treat pain.
It should never be suggested that a woman fall pregnant to treat or cure her endometriosis. This should be a personal decision based on her life circumstances, as with anyone else.
Is endometriosis cancer?
No. Endometriosis is a benign disease and although it can spread, it does not behave like cancer. There is some research that shows that women with endometriosis have a slightly higher risk of developing ovarian cancer, but this is still not well established. There have also been rare cases where endometriotic ovarian cysts became cancerous.
Who do I see if I think I have endometriosis?
Several professionals are able to help. Your GP is usually a good first call to help you assess your symptoms and the need for a specialist referral. They can also prescribe medical treatment which is sometimes all you need.
If you require surgical treatment, it is important to see a specialist Gynaecologist who has experience in endometriosis and laparoscopic surgery.
Depending on the level of endometriosis the operation can be quite complex and not everyone is trained to do it.
Physiotherapists, dietitians and fitness trainers can help with auxiliary treatments and lifestyle changes.
Resources:
Links
Endometriosis Australia: https://www.endometriosisaustralia.org/
World Endometriosis Society : http://endometriosis.ca/
Pelvic Pain: https://www.pelvicpain.org.au/
Support Groups: https://endometriosis.supportgroups.com/