Endometrial Ablation
Endometrial ablation is a minimally invasive procedure done to remove the lining of the uterine cavity called Endometrium.
Endometrial ablation is performed to treat Menorrhagia (menstrual periods with abnormally heavy or prolonged bleeding).
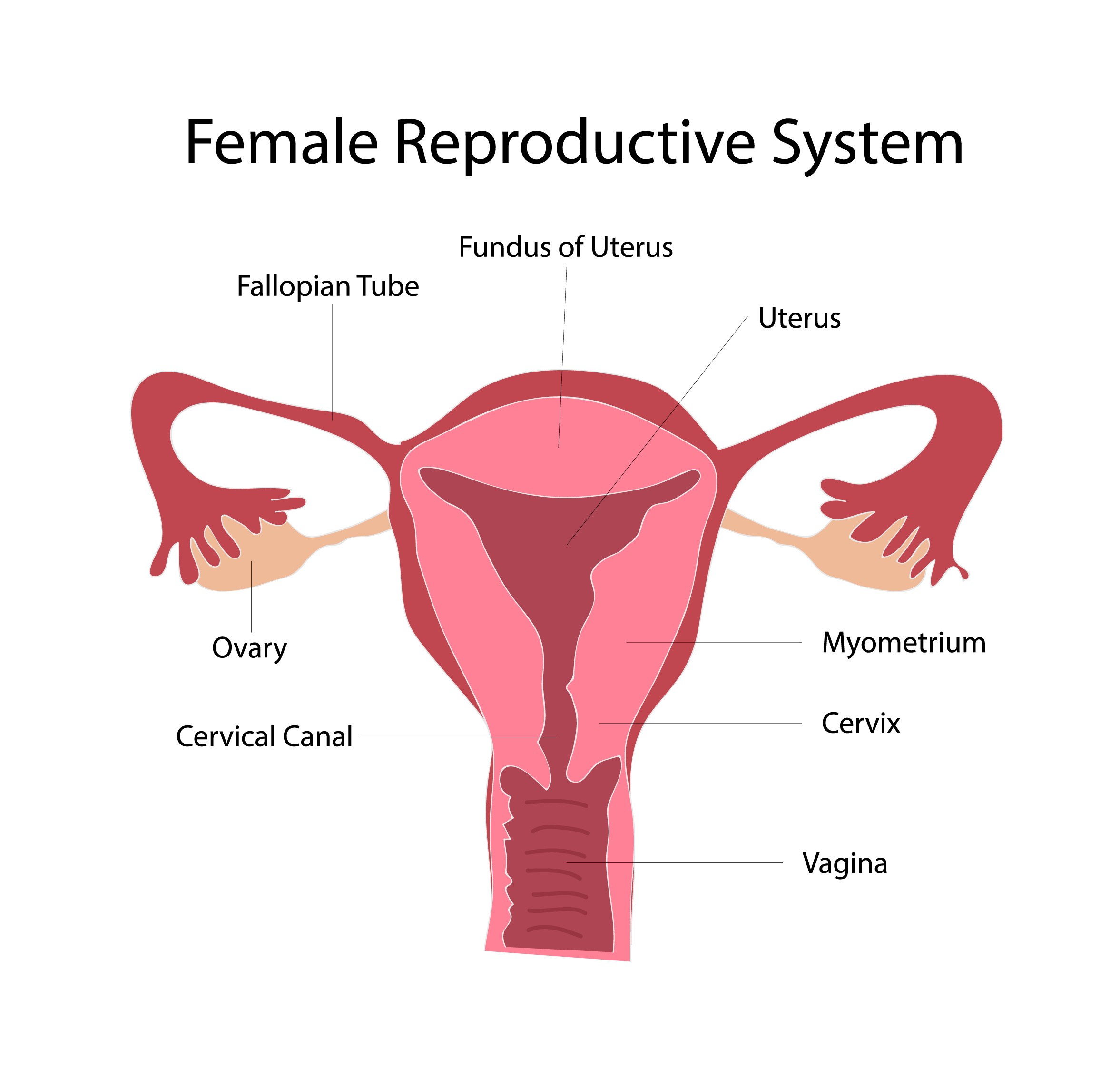
The endometrium is the layer of tissue inside the uterus. The endometrial cells have a monthly cycle of growth and collapse which is stimulated by the ovarian hormones. The number of cells and blood vessels increase over the cycle, in preparation for the implantation of the fertilised embryo. When there is no pregnancy, the endometrial cells die and shed, exposing the uterine vessels and starting the menstrual flow.
There are several reasons why a woman has increased menstrual flow. These include benign uterine growths such as fibroids or endometrial polyps, cancer of the uterus and hormonal problems.
When none of these are present and there does not seem to be a defined cause for the bleeding, the diagnosis is Dysfunctional Uterine Bleeding or DUB. About 50% of women with excessive menstrual bleeding have DUB.
There are four main groups of treatment for abnormal uterine bleeding depending on the cause:
Hormonal medication: these contain either oestrogen or progesterone or a combination of both and can be taken as tablets or injections.
Levonorgestrel IUD: Mirena is the brand name of an intrauterine device that contains a progesterone like hormone. Once inserted inside the uterus, it releases small amounts of hormones which eventually thin the endometrium and reduce the menstrual flow.
Endometrial Ablation: surgical procedure to destroy the endometrium preventing its monthly growth and shedding thus reducing the menstrual flow.
Hysterectomy: When the other measures fail, removing the uterus may be the only way to completely stop menstrual bleeding. Nowadays, only a small number of women require a hysterectomy to treat DUB as the previous less invasive options usually work quite well.
Medical treatment and the Levonorgestrel IUD are fully reversible and can be used by women who still want to preserve fertility. Endometrial ablation and certainly hysterectomy cannot be performed on women who want to preserve their ability to fall pregnant.
Frequently Asked Questions
How does endometrial ablation work?
The endometrial ablation devices deliver energy inside the uterine cavity destroying the base of the endometrial layer. This prevents the monthly proliferation of endometrial cells and subsequent shedding, reducing the amount of menstrual flow or eliminating it altogether.
How is an endometrial ablation performed?
Endometrial ablation is performed as a day procedure, meaning there is no need for overnight admission to hospital. The instruments are inserted inside the uterine cavity through the natural opening of the cervix. This means that there are no cuts or surgical incisions. Once inside, the ablation cycle starts and energy is delivered to destroy the endometrium. The duration of the procedure is only a few minutes.
Before performing the ablation, the surgeon performs a hysteroscopy to look for any abnormalities inside the uterus and to collect a sample (curetting) of endometrium for testing to make sure there were no cancerous cells. After the ablation ends, a final hysteroscopy is also done to check that the ablation was successfully done.
What are the different types of endometrial ablation available?
First generation ablation, also known as endometrial resection is performed using an instrument called a resectoscope. The surgeon uses a loop electrode or a rollerball to destroy the endometrium one small area at a time. It takes longer (20 to 40 min) and requires more surgical ability.
Second generation devices are also known as global ablation or non-resectoscopic techniques.
These have become more common because they are simpler and faster and produce the same results. In addition, the whole procedure can be done under local anaesthesia.
Several new devices have entered the market over the last few years. The main ones are:
Novasure – Bipolar radiofrequency
MEA – Microwave endometrial ablation
Thermal balloon
Cavatherm
Thermachoice
Thermablate
Hydrothermablator – Circulating hot water
Cryotherapy
How do I know which one I should have?
When compared in clinical studies, all devices seem to show similar success rates with no clear champion. The choice of device should be discussed with your doctor. Factors that influence the final decision include: product availability, hospital support and surgeon preference. In Australia, the devices that seem to produce consistent results and are most commonly used are Novasure and thermal balloon devices (Thermachoice, Cavaterm, Termablate). Novasure uses a triangular electrode that delivers bipolar radiofrequency to the endometrium. Thermal balloons, once inserted inside the uterus, are filled with fluid and inflated to the size of the uterine cavity. The fluid is then heated to high temperatures to burn the endometrium.
What is the success rate of endometrial ablation?
Success can be defined in three main different ways:
Complete elimination of periods
Patient satisfaction
No need for further treatment or surgery
Endometrial ablations have an overall very high success rate.
90% of women report being satisfied with the procedure. 50% of women will have no periods at all and about 40% will have only very light periods. 90% of women will not require any further treatment.
Endometrial ablations fail in about 10% of cases. Most of these women end up having a hysterectomy within five years.
What are the complications of the procedure?
Minor complications include:
Uterine Perforation
Haemorrhage
Infection
These occur in about 1/200 procedures and are usually easily treated without serious consequences.
A serious complication can happen if an endometrial ablation is performed after an undiagnosed uterine perforation. In this case, radiofrequency energy or high temperatures can be applied to the bowels inside the abdominal cavity. Fortunately, all modern devices incorporate a safety mechanism that checks for uterine integrity before starting the ablation and this is a very rare occurrence.
What type of anaesthesia is required?
Endometrial ablations can be performed either under local or general anaesthesia. First generation, resectoscopic techniques require general anaesthesia as the procedure can take a long time, the instruments are bigger and more manipulation of the uterus is necessary. Second generation ablations can be done either under local or general anaesthesia. General anaesthesia has the advantage of a completely pain free procedure. Women having the ablation under local anaesthesia may experience some discomfort for a few minutes, but recover quicker and leave the hospital straight away. In addition, they avoid the side effects associated with the drugs used for general anaesthesia.
Can I fall pregnant after having an endometrial ablation?
You should not fall pregnant after an endometrial ablation. The ablation itself makes falling pregnant very difficult but not impossible. If you are having an endometrial ablation it is important to use very effective contraception afterwards. There have been a few cases of pregnancy after endometrial ablation. These are all very complicated and can be life threatening for mother and baby.
What types of contraceptive can I use after an endometrial ablation?
All usual contraceptive methods can be used after an endometrial ablation, except for IUDs.
If you are used to taking the pill, progesterone injections or if you have an Implanon and wish to continue these are all fine. Otherwise, you should consider permanent contraception. The Essure and Adiana procedures can be done at the same time as the ablation. Other options are a tubal ligation or your partner having a vasectomy.
What should I expect on the days following the procedure?
Most women will experience some bleeding for up to seven days. This is usually less than an average period. Following the first few days, you should expect light brown discharge for up to six weeks.
When will I know if the procedure was successful?
It usually takes three to four months to establish a new bleeding pattern. If after six months you are still bleeding heavily, the ablation was not successful.
What if the ablation doesn’t work on reducing my bleeding?
Most companies do not recommend a second ablation if the first one has failed. Nevertheless, you should discuss this option with your doctor as there are studies showing it can be successful.
The other options discussed previously can be tried and if all fails, you may have to consider a hysterectomy.
Will the ablation change my sexual life?
Endometrial ablation has not been shown to interfere with sex and there is no reason why it should. If anything, some women report an improvement in their sexual life. This follows a reduction in symptoms which makes them more confident and increases the number of days when they feel like having sex.
Will an endometrial ablation reduce the pain I have with my periods?
Endometrial ablation has been shown to reduce the pain associated with heavy periods (Menorrhagia). The mechanisms behind this improvement and which patients will respond favourably is not clear. At present, endometrial ablation is not offered as treatment for pain.
Will an endometrial ablation reduce my PMS?
Similarly to period pain, a percentage of women who are successful in treating their heavy periods (Menorrhagia) with an endometrial ablation experience improvement in their PMS symptoms. Again, this is not well understood and endometrial ablation is not recommended as primary treatment for PMS.
Will I still need to have Pap Smears after having an endometrial ablation?
You certainly will. There are no changes to the cervix and you will continue to need regular Pap Smears like any other woman.